Creutzfeldt Jakob Disease (CJD)
- Aditya Bagwe

- Oct 24, 2022
- 5 min read
What is Creutzfeldt Jakob Disease?
Creutzfeldt-Jakob disease (CJD) is an extremely rare neurodegenerative disorder that leads to dementia and finally death within a year of the onset of the illness.
This disease affects about one in every million people per year worldwide. People with CJD typically develop symptoms later in life and may show changes in behaviour, memory troubles, lack of coordination, and vision problems.
Who discovered CJD, and where did it originate?
Creutzfeldt-Jakob disease (CJD) was named by two German doctors named Hans Creutzfeldt and Alfons Jakob who studied the disease in the 1920s.
Friedrich Meggendorfer is credited as having first described a familial case of CJD in 1930, a case which was later confirmed by genetic analysis. Kuru, a prion disease acquired by cannibalism, was discovered in 1957. The disease was observed to have symptoms comparable to scrapie, a transmissible disease of sheep.
Variant CJD was first identified in March 1996 in the UK, when 10 cases of a new disease with neurological symptoms were reported and soon associated with the Bovine Spongiform Encephalopathy (BSE), “mad cow”-disease.
MRI Scans of patients with Creutzfeldt-Jakob disease

sourced from:https://en.wikipedia.org/wiki/Creutzfeldt%E2%80%93Jakob_disease
Comparison of the brain affected by CJD and one not affected by it (control)

Can CJD be dormant?
Variant CJD has an average incubation time of 30 years or longer because the prions are passing from infected cattle to humans rather than from human to human. But when the person gets infected by CJD, there is quick progression of the disease that leads to deterioration of the mental condition of the patient along with extremity weakness, blindness, and eventually, the patient may go into a coma.
How does CJD occur?
CJD is believed to be caused by an abnormal isoform of a cellular glycoprotein known as the prion protein. In CJD, the prion protein (PrPC) mutates into an abnormal form known as PrPSc. This change in the protein causes steady and irreversible neurological destruction in the brain that is ultimately fatal.
These abnormal prions accumulate at high levels in the brain, which causes the brain to slowly shrink and the tissue to fill with holes until it resembles a sponge.
sourced from: https://www.youtube.com/watch?v=xQtp2zMd9iY&ab_channel=SotonBrainHub and https://www.epainassist.com/brain/creutzfeldt-jakob-disease-or-cjd
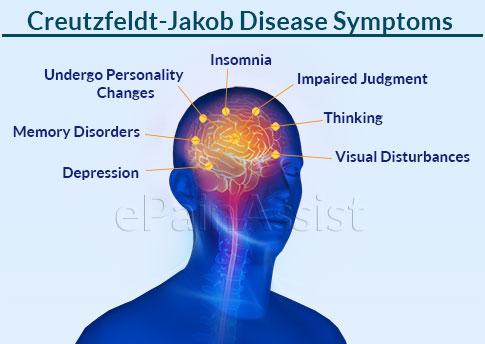
What are the symptoms of CJD?
Loss of intellect and memory
Changes in personality
Loss of balance and coordination
Slurred speech
Vision problems and blindness
Progressive loss of brain function and mobility
How can CJD be diagnosed?
The detection of CJD has evolved over the years with the help of advancements in technology.
1. Brain biopsy (1970s): Vacuolated empty spaces in the neuropil could be seen as neuronal loss, and gliosis had occurred.
2. Electroencephalogram (EEG) test (1980s): Periodic, sharp and slow wave complexes could be observed from the graph formed.
3. Extracting and analyzing cerebrospinal fluid (1990s): elevated levels of protein 14 3 3 were detected in the samples from the brain and spinal cord.
4. MRI scan(2000s): Abnormally high signals transmitted from the basal ganglia, thalamus, and cortical areas.
5. Real-Time Quaking-Induced Conversion(2010s): Detection of a mutated prion protein called PrPSc.

What are the different types of CJD?
The length of illness depends on the type of CJD involved, and there are currently four main types that we know of;
1. Sporadic CJD: This was first described in the 1920s and remains the most common form of the disease as it accounts for 85% of all CJD cases today. It affects approximately one person in a million per year, and there are around 50 cases annually in the UK. Its cause remains unclear, but it does not seem to be linked to cattle BSE or so-called "mad cow disease."
2. Genetic (Familial or Inherited) CJD: This form is rarer than sporadic CJD, as it accounts for 10-15% of all cases. There is a family history of the problem in these cases, so it appears to be an exclusively inherited condition. It kills less than 5 people each year in the UK.
3. Iatrogenic CJD: This form is caused by a medical accident or contamination, such as through infected surgical instruments. This is a very rare incident, so iatrogenic CJD accounts for 1% of all cases.
4. Variant CJD: The variant CJD is most likely caused by consuming meat from a cow that has “mad cow disease," which is a similar prion disease to CJD. This can be prevented by stopping meat from infected cattle from entering the food chain.
Is there any treatment for CJD?
As of now, there is no cure for CJD; the treatments are used to relieve symptoms and make patients feel as comfortable as possible.
For example, psychological symptoms such as anxiety and depression are treated with sedatives and antidepressants.
Muscle jerks or tremors can be treated with medications like clonazepam and sodium valproate.
Pain experienced can be relieved by opiate-based painkillers.
Can CJD be prevented?
Even though CJD is rare, it can often be difficult to prevent. This is because most cases can occur spontaneously without any reason, such as Sporadic CJD. Familial CJD cannot be prevented as it is caused by a fault in the inherited genes.
Although sterilization can prevent bacteria and viruses from spreading, it is ineffective against the infectious prion protein that causes CJD. But the tightened guidelines on reusing surgical equipment mean that the spread of iatrogenic CJD is rare.
There are also strict measures and regulations in place to prevent the spreading of CJD through the food chain or through the blood supply during blood transfusions.
Conclusion
Since CJD has no cure, the medicine used is for easing the symptoms of depression, insomnia and problems with movement. The best option is always to prevent the contraction of the disease. This prevention varies according to the type of CJD one can possibly be diagnosed with. Most types of CJD infections can be avoided by following strict protocols in hospitals and following appropriate health and nutrition guidelines.
Written By: Aditya Bagwe
Glossary:
Neurodegenerative disorder- A type of disease in which cells of the central nervous system stop working or die.
Isoform- A protein that has the same function as another protein but which is encoded by a different gene and may have small differences in its sequence.
Prions- Misfolded proteins that have the ability to transmit their misfolded shape onto normal variants of the same protein.
Brain biopsy- It is the removal of a small piece of brain tissue for the diagnosis of abnormalities of the brain
EEG test- An electroencephalogram (EEG) is a recording of brain activity. During this painless test, small sensors are attached to the scalp to pick up the electrical signals produced by the brain.
Cerebrospinal fluid- A clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord
Insomnia- A common sleeping disorder where the patient has difficulty in falling asleep and as a result they feel fatigued very often.
Bibliography:
Balonwu, Vivienne. “Creutzfeldt Jakob Disease.” Health and Medical , Free Health & Medical Information Online, 13 July 2015, https://www.viviennebalonwu.com/2015/07/creutzfeldt-jakob-disease-cjd.html.
Stanclift, Caroline, and Jennefer Kohler. “Creutzfeldt Jakob Disease.” Rare Disease Database, NORD (National Organization for Rare Disorders), 14 June 2021, https://rarediseases.org/rare-diseases/creutzfeldt-jakob-disease/.
Bauer, Juliet. “Creutzfeldt Jakob Disease.” NHS Choices, NHS, 7 September 2021, https://www.nhs.uk/conditions/creutzfeldt-jakob-disease-cjd/.
Zerr, Inga, and Dr Zerr. “Laboratory Diagnosis of Creutzfeldt–Jakob Disease.” Creutzfeldt Disease, The NEW ENGLAND JOURNAL of MEDICINE, 7 Apr. 2022, https://www.nejm.org/doi/10.1056/NEJMra2119323?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed.
Mead, Simon, and Fabrizio Tagliavini. “Diagnosis of Creutzfeldt-Jakob Disease.” Diagnosis of Creutzfeldt-Jakob Disease - an Overview | ScienceDirect Topics, Science Direct, 10 Jan. 2018, https://www.sciencedirect.com/topics/medicine-and-dentistry/diagnosis-of-creutzfeldt-jakob-disease.
Kerkar, Pramod. “Creutzfeldt-Jakob Disease or CJD: Categories: Symptoms: Diagnosis: Causes: Prognosis.” Epainassist, Pain Assist Inc., 19 June 2018, https://www.epainassist.com/brain/creutzfeldt-jakob-disease-or-cjd.






Commentaires